Professional Medical Billing Services That Deliver Results
We understand that every claim represents the financial foundation that keeps your practice running and allows you to focus on delivering exceptional patient care. Our dedicated billing teams treat your revenue with the same attention and expertise you provide to your patients.
Take the first step toward financial peace of mind.
CALL (386) Billing ( 386 245 5464)
Medical Billing Services That Maximize Your Revenue!
Do you know approx $125 billion slips away every year in the U.S. because of billing errors? Yet most of it is recoverable!
At Health and Billing, we combine advanced technology with expert oversight to help practices recover more revenue, reduce rejections, and speed up reimbursements
- 100% HIPAA-compliant processes that safeguard your practice.
- Optimized claim accuracy to cut rejections and denials.
- Accelerated payment cycles that improve your cash flow.
- Revenue-focused strategies for long-term financial stability.
Start Optimizing Your
Billing Today.
What Health and Billing Offers?
We cover every stage from patient intake and eligibility verification to medical coding, claims submission, denial management, patient collections, and financial reporting. With us, your billing isn’t just managed. It is optimized for YOUR growth and MORE revenue!

Complete RCM Coverage
A 360° solution that ensures no revenue is left behind!

98–99% Clean Claim Rate
Thus, drastically reducing rejections.

20–35% Revenue Uplift

AI-Driven Accuracy

Full Legal & Data Compliance
- HIPAA (Health Insurance Portability and Accountability Act)
- HITECH Act for secure health IT usage
- SOC 2 Type II certified processes
- OIG Exclusion Checks for regulatory safety
- CMS guidelines for Medicare/Medicaid compliance

Technology-Enabled Solutions
- eClinicalWorks
- Epic Resolute

Faster Reimbursements

Performance Metrics & Reporting

Bills Collection & 24/7 Expert Support

KPI Dashboard
Schedule a Free Discussion!
Health & Billing
WHO WE SERVE?
- Solo and multi-provider practices
- Small clinics through large hospitals
- Specialty centers (e.g., imaging, ambulatory surgery)
- Labs, FQHCs, and DME providers
- Practices across more than 50 medical disciplines


Did you know the average denial rate in healthcare is 10%?
Stop leaving money on the table and start getting paid what you deserve!
Our Technology-Driven Approach
Credentialing & Enrollment
Eligibility & Pre-Authorization
Medical Coding & Charge Entry Services
Claim Submission & Scrubbing
Denial Management & Appeals
Accounts Receivable (A/R) Recovery
Patient Billing & Collections
Advanced Analytics & Reporting
Quarterly Audits & Fee Schedule Optimization
Seamless EHR & Practice Management Integration
Our Technology-Driven Approach

Credentialing & Enrollment
Eligibility & Pre-Authorization
Medical Coding & Charge Entry Services
Claim Submission & Scrubbing

Denial Management & Appeals

Accounts Receivable (A/R) Recovery
Patient Billing & Collections
Advanced Analytics & Reporting
Quarterly Audits & Fee Schedule Optimization

Seamless EHR & Practice Management Integration
Our Technology-Driven Approach
-
Credentialing & Enrollment
Get listed with all major payers quickly and avoid costly delays. -
Medical Coding & Charge Entry Services
Certified coders (CPC, CCS-P) with deep specialty expertise use AI-driven checks for CPT, ICD-10, and HCPCS accuracy. -
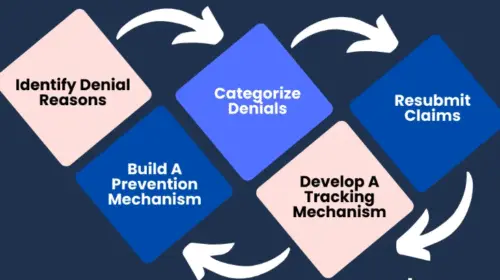
Denial Management & Appeals
Denials are analyzed, corrected, and resubmitted within 24–48 hours. Complex cases are appealed aggressively. -
Patient Billing & Collections
Clear statements, online payment portals, and compassionate patient support reduce friction and improve collections. -
Quarterly Audits & Fee Schedule Optimization
Identify underpayments, benchmark against peers, and adjust your fees for maximum reimbursement.
-
Eligibility & Pre-Authorization
Real-time insurance verification ensures coverage before services are delivered. -
Claim Submission & Scrubbing
Electronic claim submission (ANSI X12-837) with 3-layer scrubbing for maximum first-pass acceptance. -
Accounts Receivable (A/R) Recovery
We follow up relentlessly, recovering aged claims—even those 120+ days old. -
Advanced Analytics & Reporting
Dashboards with KPIs such as denial rates, net collections, payer mix, and cost-to-collect. -
Seamless EHR & Practice Management Integration
Works smoothly with top EHRs like Epic, Athenahealth, Kareo, AdvancedMD, eClinicalWorks, and Allscripts.
Why Outsource Medical Billing Services?
Minimize your Administrative Burden.
With Improven Accuracy
FAQs
We provide end-to-end Revenue Cycle Management (RCM). From eligibility verification, medical coding (CPT, ICD-10-CM, HCPCS Level II), claim scrubbing, denial management, AR recovery, to patient collections, we are an all-in-one solution.
Yes, 100%. All workflows follow HIPAA, HITECH, SOC 2, CMS, and OIG standards, ensuring secure PHI handling and audit-ready billing practices.
Our KPI dashboards track AR per payer, copays, bill statuses, and revenue trends. Performance metrics allow actionable insights for cash flow optimization and scalable practice growth.
Yes. From solo practitioners to multi-location practices, our RCM platform scales while maintaining clean claims, compliance, and performance oversight.
Through AI-powered claim validation, predictive denial analysis, and payer-specific edits, we achieve 98–99% clean claims, reduce denials below 2%, and recover up to 35% more revenue.
Our Certified coders (CPC, CCS-P) ensure specialty-specific coding accuracy. We support many specialties, including Psychiatry & Mental Health, Neurology, Anesthesia & Pain Management, Cardiology, Internal Medicine / Family Medicine, Urgent Care, and more.
We automate insurance eligibility checks, co-pay collection, and patient balance reminders to reduce AR days. Patients receive transparent statements, improving collections without friction.
Most practices observe improved first-pass claim acceptance, reduced denials, and faster reimbursements within 60–90 days.

